Imagine this: It’s mid-afternoon, you’ve skipped lunch (or had a sugary snack), and suddenly you feel jittery, anxious, maybe a bit shaky. A thought pops: “Did I just mess up work? What if they notice my hands trembling?” Within moments, that turns into “I’m incompetent,” or “Everyone hates me.” You feel trapped, overwhelmed—emotional trauma over something small.
That’s one blood sugar battle waging war inside. This post is about how blood sugar fluctuations can exacerbate anxiety, depression, panic, or negative thinking—and what you can do about it as both a Govt.Recognized Counsellor & Mind Healer.
also read: why digital conversations arekilling real connection?
You may think: “Am I just overthinking? Is this an anxiety disorder?” Many people feel guilt or shame: “I must be weak, I must be going crazy.” But in fact, your body (and brain chemistry) is fighting a silent war.
also read: how to read body language signs indaily life?
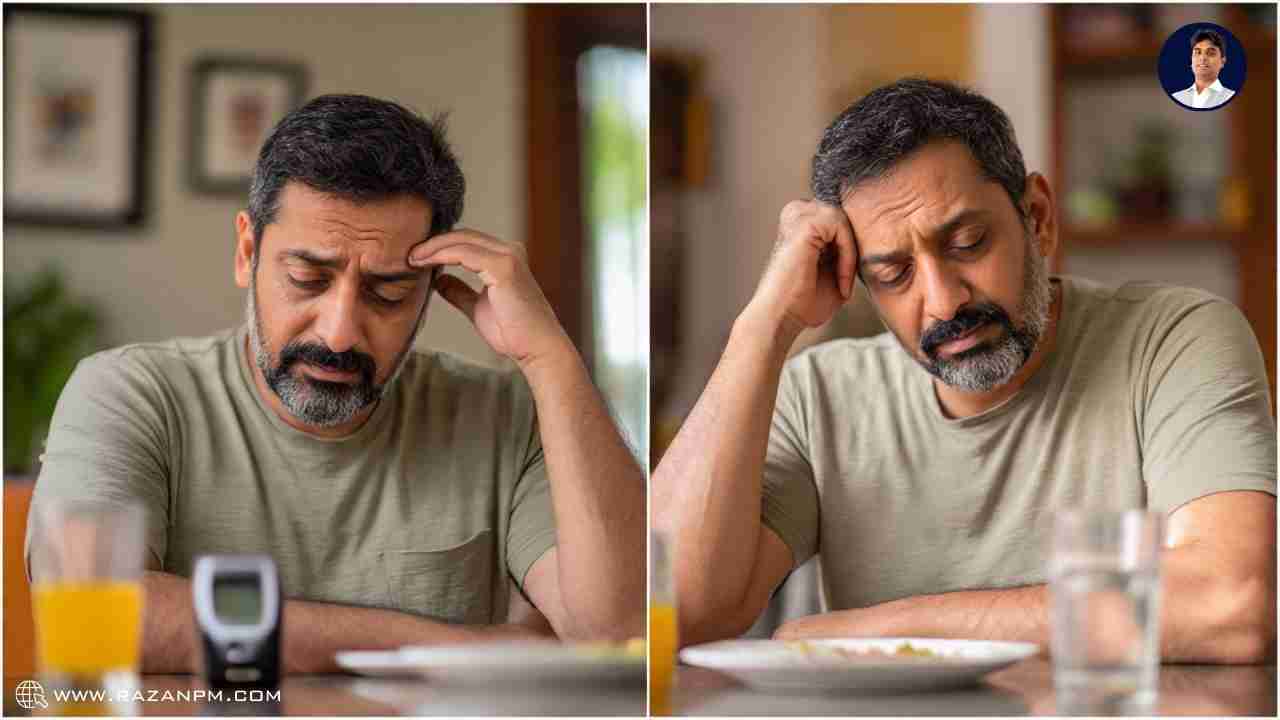
These are especially seen in hypoglycemia (low blood sugar) episodes—where your body triggers stress responses to bring glucose back up.
Also, if your blood sugar fluctuates a lot (glycemic variability), that itself is correlated with higher incidence of anxiety and depression.
also read: 8 signs of hidden depression incancer survivors
From a DSM-5 perspective (and ICD-11), psychological symptoms like anxiety disorders or mood disorders may sometimes be “Anxiety disorder due to another medical condition” if a medical condition directly causes or exacerbates the anxiety.
So clinically, an astute psychologist or psychiatrist will assess whether symptoms are partly driven by metabolic/medical factors (blood sugar), not just psychological origin.
also read: 12 behaviors that reveal a man issexually frustrate

A large cohort study (151,814 individuals) found that higher long-term fluctuations in blood glucose were associated with higher incidence of diagnosed depression and anxiety (using ICD codes).
When cells resist insulin, brain metabolism changes. Stanford researchers found insulin resistance doubles the risk of major depressive disorder.
Stanford Medicine
In a study of US adults, every additional 100 grams/day of dietary sugar was linked to a 28% higher prevalence of depression.
Also, systematic reviews suggest sugar intake leads to mood swings through both glycemic effects and inflammation in the brain.
Hypoglycemia triggers epinephrine release (stress hormone) causing anxiety, shaking, and psychological symptoms.
Chronic high blood glucose can shrink brain connections, affect connectivity, and impair cognition.
Harvard Medical School
Depression and diabetes amplify each other: depression may lead to poor diet, inactivity, weight gain → insulin resistance; and diabetes may contribute to depression.
All this tells us: blood sugar is not just about physical health. It deeply affects mental health, mood regulation, cognition, and emotional resilience.
also read: 9 hidden signs she misses physicalaffection
Now let me take you behind the scenes. As a Govt.Recognized Counsellor & Mind Healer, I used to have sessions where clients with mood swings, “panic out of nowhere,” or negative spirals had no “classic diagnosis.” They were frustrated that therapy sometimes didn’t help enough. One evening, a client—a young software engineer—burst into tears: “Yesterday my glucose dropped; I felt so anxious, I believed everyone was judging me at work. It was irrational, but I couldn’t stop the fear.”
also read: why gen z cant sleep anymore and theoverthinking trap?
I felt the emotional weight in that room: he thought he was “losing it,” but really he was being hijacked by his physiology. I started reading neuroendocrinology, nutrition science, psychoneuroimmunology—and merged that with NLP-based patterns. Over months, I experimented in my own life with blood sugar stabilization and noticed my own mood swings, irritability, mental chatter reduced dramatically.
Then I tried this in therapy: combining blood sugar stabilization + NLP reframing + cognitive tools. Clients started reporting “I used to spiral at 3 pm, now I catch it and stop it.” Many tears of relief followed—when people realize they are not “mad,” not “crazy,” but simply out of metabolic balance.
also read: 12 things women do when theyre touchdeprived

Here’s something you can start today, by yourself. No guru, no 10-week course required.
When to do it: Mid-afternoon (say 2:30–3:30 pm), or whenever you feel shaky, irritable, brain foggy, anxious, or having negative thoughts escalating.
1. Before eating, pause: take 3 deep breaths.
2. Say to yourself: “I am giving my brain fuel, I only need a moment to breathe.”
3. Visualize your brain lighting up with clarity and calmness.
4. Notice how your thoughts shift—are you less harsh, less catastrophic?
This combo gives stable glucose (protein + fat slows absorption), prevents big spikes and crashes, and gives a psychological “anchor” (pause + affirmation) to interrupt a negative spiral.
Try this for 3 weeks, every day when you feel that mid-journey slump. Note your mood before and 30 – 60 min after.
People often see improvement: fewer catastrophes, less agitation, a calmer mind.
also read: why gen z cant sleep anymore and theoverthinking trap?
This mini step is a doorway, not the whole path. Behind it lie structured protocols:
To fully recover emotional balance in relationship to your metabolism, one needs a guided, personalized plan. A blog can’t tailor all of it—but a therapeutic process can.
also read: why couples feel unheard and how tofix it fast
If reading this stirred something familiar in your heart—if you’ve felt that shadow of negative thoughts triggered by nothing, or fear heaving in your chest after a sugar crash—you don’t have to walk this path alone.
Let’s work together—body + brain + belief. Let me help you map your metabolic triggers, recalibrate your inner narrative, and restore emotional harmony.
If this resonates, feel free to book a 1:1 consultation here. We can unravel your unique pattern, step by step, in a safe, compassionate space—no judgment, only collaboration.
👉Begin Your Journey with a 1 on 1 Consultation
👉Begin Your Journey with a 1 on 1 Consultation

A: Fluctuating blood sugar affects brain chemistry, especially serotonin and cortisol, which control mood and energy. Spikes or crashes can trigger anxiety, irritability, or depression.
A: Yes. Low blood sugar (hypoglycemia) activates stress hormones like adrenaline, causing symptoms similar to panic attacks — shakiness, racing heart, and fear.
A: Eat balanced meals with protein, fiber, and healthy fats. Avoid skipping meals or eating too much sugar. Try the “Balanced Snack Rescue Protocol” from the blog for quick relief.
also read: why generational habits shape how weescape?
A: Studies show high or unstable glucose levels (glycemic variability) are linked to a greater risk of depression and brain fatigue due to inflammation and hormonal imbalance.
A: Therapy and NLP help you identify triggers, manage emotional responses, and reframe negative thought loops — combining mind science with body awareness for long-term calm.
also read: 8 emotional changes in women withoutintimacy
